UNIGE researchers have discovered that a medication commonly used to treat herpes can combat an antibiotic-resistant bacterium by disrupting its defense mechanisms.
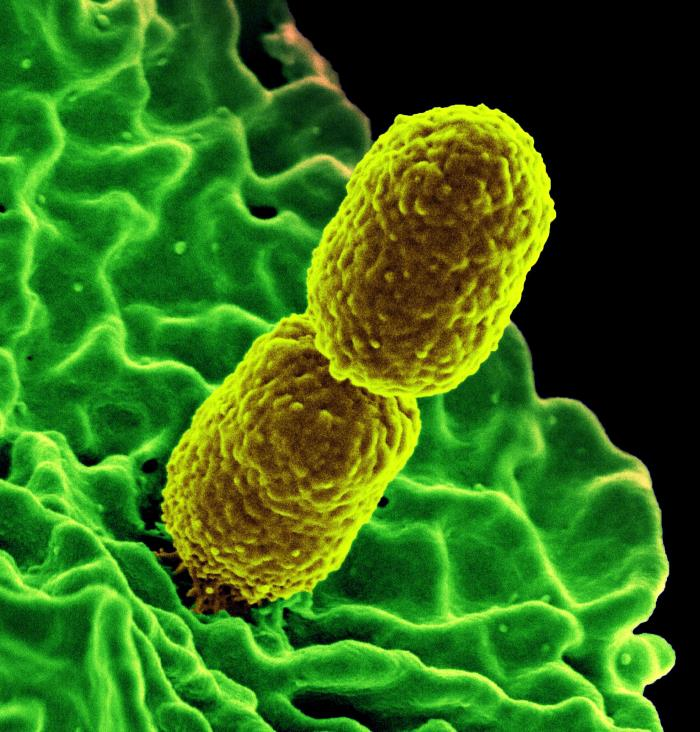
Antibiotic resistance, or the ability of bacteria to develop resistance to treatment with antibiotics, has become a major concern for global health. The World Health Organization (WHO) considers it one of the greatest threats to health. The overuse of antibiotics has contributed to the emergence of antibiotic-resistant bacteria, which can cause serious illness and death. One example of an antibiotic-resistant pathogen is Klebsiella pneumoniae, a bacterium commonly found in hospitals and known for its virulence. Without effective treatment options, we could see a resurgence of diseases such as pneumonia and salmonella, which were once easily treated with antibiotics.
Researchers at the University of Geneva (UNIGE) have found that edoxudine, an anti-herpes molecule developed in the 1960s, can disrupt the protective surface of Klebsiella bacteria and make them more vulnerable to being eliminated by immune cells. The researchers’ findings were recently published in the journal PLOS ONE.
Klebsiella pneumoniae causes many respiratory, intestinal, and urinary tract infections. Due to its resistance to most common antibiotics and its high virulence, some of its strains can be fatal for 40% to 50% of infected people. There is an urgent need to develop new therapeutic molecules to counter it.
“Since the 1930s, medicine has relied on antibiotics to get rid of pathogenic bacteria,” explains Pierre Cosson, professor in the Department of Cell Physiology and Metabolism at the UNIGE Faculty of Medicine, who led this research. “But other approaches are possible, among which trying to weaken the bacteria’s defense system so that they can no longer escape the immune system. This avenue seems all the more promising as the virulence of Klebsiella pneumoniae stems largely from its ability to evade attacks from immune cells.”
An amoeba as a model
To determine whether or not the bacteria were weakened, the UNIGE scientists used an experimental model with surprising characteristics: the amoeba Dictyostelium. This single-cell organism feeds on bacteria by capturing and ingesting them, using the same mechanisms that immune cells use to kill pathogens. “We genetically modified this amoeba so that it could tell us whether the bacteria it encountered were virulent or not. This very simple system then enabled us to test thousands of molecules and identify those that reduced bacterial virulence,” explains Pierre Cosson.
Weakening the bacteria without killing them
Developing a drug is a long and expensive process, with no guarantee of results. The UNIGE scientists, therefore, opted for a quicker and safer strategy: reviewing existing drugs to identify possible new therapeutic indications.
The research team evaluated the effect on Klebsiella pneumoniae of hundreds of drugs already on the market, with a wide range of therapeutic indications. A drug developed to combat herpes, edoxudine, proved particularly promising.“By altering the surface layer that protects the bacteria from their external environment, this pharmacological product makes it vulnerable. Unlike an antibiotic, edoxudine does not kill the bacteria, which limits the risk of developing resistance, a major advantage of such an anti-virulence strategy,” says the researcher.
Although the effectiveness of such a treatment in human beings has yet to be confirmed, the results of this study are encouraging: edoxudine acts even on the most virulent strains of Klebsiella pneumoniae, and at lower concentrations than those prescribed to treat herpes. “Sufficiently weakening the bacteria without killing them is a subtle strategy, but one that could prove to be a winner in the short and long terms,” concludes Pierre Cosson.
Reference: “5-ethyl-2’-deoxyuridine fragilizes Klebsiella pneumoniae outer wall and facilitates intracellular killing by phagocytic cells” by Estelle Ifrid, Hajer Ouertatani-Sakouhi, Tania Jauslin, Sebastien Kicka, Gianpaolo Chiriano, Christopher F. Harrison, Hubert Hilbi, Leonardo Scapozza, Thierry Soldati and Pierre Cosson, 31 October 2022, PLOS ONE.
DOI: 10.1371/journal.pone.0269093